|
CT血管造影(CTA) 20年的发展之路(连载三)——CT血管造影术对于临床的贡献:急性主动脉综合症(AAS)——新的知识重新定义疾病分类
作者:Geoffrey D. Rubin, MD
作者单位:Duke Clinical Research Institute, 2400 Pratt St 本文发表于:Radiology: Volume 271: Number 3—June 2014 radiology.rsna.org 翻译:郑颖;校对:张帅、陆伟;整理:梁军 
上期回顾: 本综述介绍了CT血管造影术的起源与发展。 本期内容:
CT血管造影术对于临床的贡献:急性主动脉综合症(AAS)——新的知识重新定义疾病分类。 AAS(急性主动脉综合症)是指一系列急性的、威及生命的主动脉异常病变,它以突然出现的剧烈胸部或背部疼痛为主要特征。CT血管造影(CTA)不仅彻底改变了对AAS的诊断与治疗,而当扫描采集与心电图(ECG)同步时,则从根本上更易理解AAS的症状,它正成为对AAS进行诊断、定性、制定治疗计划的一项优越技术。
CTA对于临床应用的贡献 Contributions of CT Angiography to Clinical Practice
由于巨大的技术进步,CTA已经发展到可以为心血管疾病的诊断与治疗方面提供非常重要的见解。虽然许多CTA的应用改变了临床诊疗的标准并且值得不断的精细化,但我们还是选择特别关注的三个方面,CTA拓宽我们对人类血管性疾病(急性主动脉综合征(AAS)和外周动脉疾病)的理解,其中有指导疾病治疗方面引导(主动脉内支架置入和经皮主动脉瓣膜置换)的新策略,以及这新技术提供进一步优化(对冠心病的诊疗)的承诺。 As a result of tremendous technologic developments, CT angiography has evolved to provide important insights into cardiovascular disease diagnosis and management. While there are many applications of CT angiography that have transformed the standard for clinical care and are worthy of detailed elaboration, we have chosen to focus specifically on three areas in which CTangiography has expanded our under- standing of human vascular disease & #40;AAS and peripheral arterial disease& #41;, in which it has guided new strategies in disease management & #40;aortic endograft deployment and transaortic valve implantation& #41;,and in which new CT techniques offer promise for further refinements & #40;coronary heart disease& #41;.
急性主动脉综合征(AAS):新知识重新定义疾病分类 Acute AorticSyndromes: New Knowledge Redefining Disease Acute Acute Aortic Syndromes: New Knowledge Redefining Disease Classification
AAS是指一系列急性的,威及生命的主动脉异常,以突然出现的剧烈胸部或背部疼痛为特征& #40;28& #41;。 AAS refers to a spectrum of acute, life-threatening abnormalities of theaorta characterized by an abrupt onset of in- tense chest or back pain& #40;28& #41;.
CT血管造影(CTA)不仅彻底改变了对AAS的诊断与治疗(29),而且当扫描采集与心电图(ECG)同步时,就从根本上更易理解AAS的症状(30),它正成为对AAS进行诊断、定性、制定治疗计划的一项优越技术。除了克服因升主动脉搏动所导致误诊与虚假的病理结果(30,31),心电图的同步能对主动脉根部及相关的冠状动脉窦进行正确评价。 CT angiography has not only revolutionized the diagnosis and management ofcases of AAS& #40;29& #41;, but when acquired with electrocardiographic & #40;ECG& #41; synchronization has fundamentally advanced our understanding of these conditions& #40;30& #41;, becoming the preeminent technique for the diagnosis,characterization, and treatment planning of AAS. In addition to overcoming ascending aortic pulsation artifacts that have resulted in both missed andspurious pathologic findings & #40;30,31& #41;, ECG synchronization enables assessment of aortic root and coronary ostial involvement.
无运动伪影干扰的图像能够可靠的识别原发性内膜撕裂的位置,夹层的位置和程度,以及所累及的分支动脉,这对指导治疗非常重要(图2,3)。在病理学上一些常见但至今无法可视化的征象(例如,壁间血肿【IMH】内的血池与侧支血管(32))与在活体诊断图像上以前认为无法探测的细微病变能力(即,局限性夹层(30,33))等已由CT血管造影(CTA)技术引导并发展出了急性主动脉病变新的分类方法(34)。 Motion-free images enable reliable identification of the site of the primary intimal tear, location and extent of dissection flaps, and branch-artery involvement— features important in guiding therapy & #40;Figs 2, 3& #41;. Visualization of hitherto un- known but common pathologic features(eg, blood pools and side branch communications within an intramural hematoma [IMH](32))and theability to detect subtle lesions previously deemed inaccessible to in vivodiagnostic imaging(ie, limited dissection(30,33))have allowed CT angiography to lead the way to new classifications of acute aortic lesions.
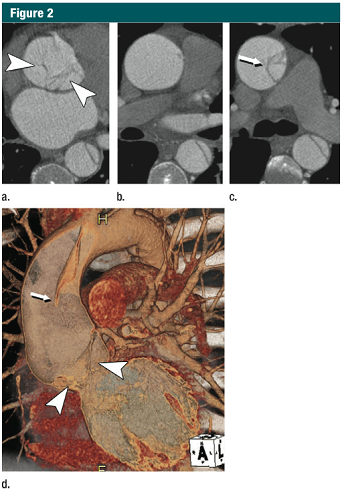
图2 45岁,男,A型急性主动脉夹层 (a-c)CT横断位图像: (a)主动脉根部水平不规则线样阴影(箭头) (b)升主动脉中段没有夹层皮瓣 (c)升主动脉远端可见夹在真、假腔之间的夹层皮瓣(细箭) (d)VR重建展示夹层,近端夹层撕裂皮瓣下垂向下通过主动脉瓣膜(箭头)。细箭所指远端升主动脉的夹层皮瓣。在无ECG门控的时候,这些细微的发现并不可见。(转载、许可、引用30) 
图3 升主动脉局限性内膜撕裂 (a)上方:无心电门控的CTA显示升主动脉运动伪影,模糊;下方:12小时后,心电门控 CTA示:升主动脉近端内膜皮瓣& #40;箭头& #41;,伴随一个侵蚀边缘的局限性内膜撕裂。局限性内膜撕裂的边缘(大箭头)和主动脉壁破坏形成的突起(小箭头)清晰可见。这些微妙细节如果没有使用心电门控是不可见的。 (b)VR重建显示腔内一侧150px长的损伤。一个小的破损皮瓣(细箭)代表撕裂的起始端,并一直延伸到主动脉弓的近端。虚线,代表撕裂的边缘。(转载,许可,引用24。)
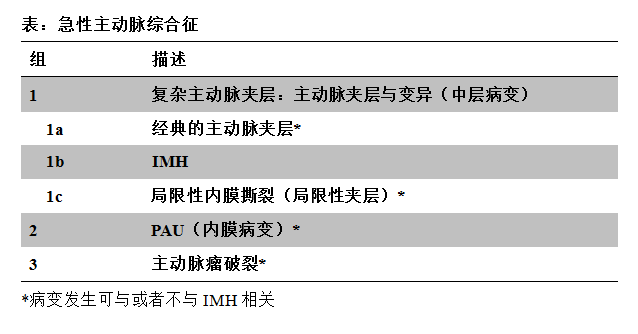
传统的AAS分为主动脉夹层、IMH与穿透样动脉粥样硬化性溃疡(penetrating atherosclerotic ulcer,PAU)(34,35),现在可通过CTA分析重新定义。 The traditional "classification" of AAS into aortic dissection, IMH, and penetrating atherosclerotic ulcer & #40;PAU& #41; & #40;34,35& #41; can be refined through analysis of CT angiography.
CTA技术带来的最重要的见解之一是,IMH除了发生在多种典型的主动脉夹层外,还可以发生在任何急性主动脉异常中,包括全部各种夹层,穿透样动脉粥样硬化性溃疡,以及任何病因(动脉粥样硬化、相关的连接组织、霉菌、甚至创伤后、医源性以及非医源性因素)(图4)导致的主动脉瘤破裂。 Perhaps one ofthe most important insights gleaned from CT angiography is that in addition toits classic deion as a variant of aortic dissection, IMH may be seen inassociation with virtually any acute aortic abnormality, including the entirespectrum of dissection variants, PAUs, and rupturing aortic aneurysms of anyetiology & #40;atherosclerotic, connective tissue-related, mycotic, and even posttraumatic, iatrogenic or noniatrogenic& #41; & #40;Fig4& #41;. 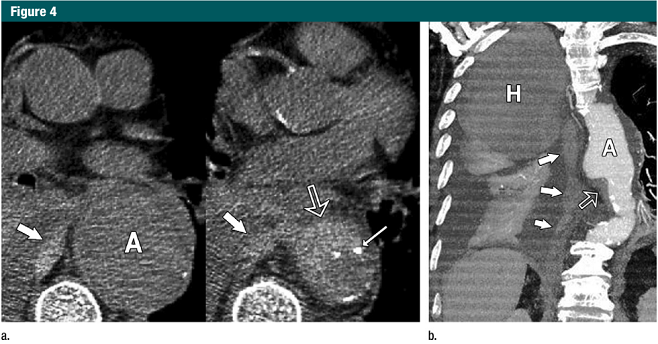
图4:合并IMH的动脉瘤破裂 (a)横断位CT部分展示150px的降主动脉瘤(A)。IMH(开放箭头)在动脉瘤的下缘,伴有内膜钙化(细箭头)与中纵膈内持续出血(粗箭头)。 (b)斜位薄层MIP的CTA成像显示IMH(开放箭头)在动脉瘤(A)下缘,长条状的血液(实心箭头)贯穿纵膈扩展到胸膜腔,一个大的血肿(H)占据了右半胸廓的近一半位置,与低密度的胸腔积液和强化的右肺膨胀不全有明显的区别。(转载、许可、引用24)
因此,IMH可以被认为是伴随急症如主动脉夹层,PAU,和主动脉瘤破裂的影像征象,而非目前通常所认为的IMH只是AAS一个独特“条件”的征象(34,35)。而且,主动脉夹层和PAU,与主动脉瘤破裂的IMH伴随征象也引出了这样一个问题:为什么AAS不包括主动脉瘤破裂(30)。 Thus, IMH might be more appropriately classified as an imaging marker of acuity associated with aortic dissection, PAU, and rupturing aneurysm rather than thecurrently in vogue characterization of IMH as a distinct “condition” of AAS& #40;34,35& #41;. Moreover, the association of IMH with both the classic AAS conditions of aortic dissection and PAU and with rupturing aortic aneurysm introduces the question as to why rupturing aortic aneurysms are not included as AAS & #40;30& #41;.
由ECG门控的CTA揭示了另一个完全不同的概念,它认为AAS是一系列疾病的表现,由三个主要的病理过程引起:第一组,血管中层病变导致的主动脉夹层和其变异;第二组,PAU,是动脉粥样硬化进展的表现,然后是内膜病变;第三组,主动脉瘤破裂,其临床表现与主动脉夹层和PAU明显不同(表)(30)。注意,IMH并不是这个分类的一部分,因为它可以伴随以上三个病理过程,是急性过程的指征。 An alternative concept informed by observations from ECG-gated CT angiography regards AAS as a spectrum of disease manifestations caused by three main pathologic processes: group 1, aorticdissection and its variants resulting from a diseased media; group 2, PAU,which is a manifestation of advanced atherosclerosis and thus a disease of the intima; and group 3, rupturing aortic aneurysms, as the clinical presentationis indistinguishable from aortic dissection and PAU & #40;Table& #41;(30). Note that IMH is not part of this classification as it may be associated with any of the three main categories asan indicator of an acute process. 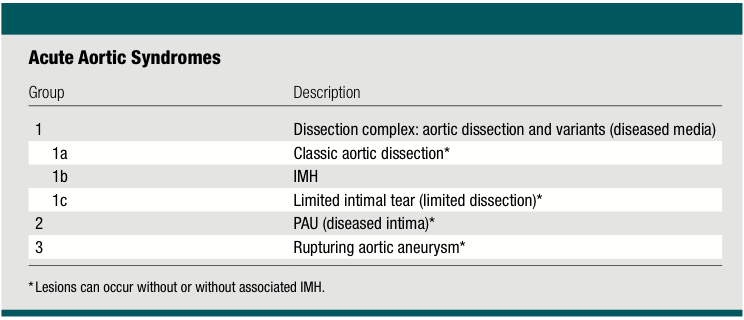
由于有着共同的病理改变,代表主动脉夹层及其变异的第一组病变都是动脉壁中层病变。典型夹层的征象是主动脉壁内形成一个通道或者假腔,后者通过撕裂的内膜与真腔分离(图2)。 Group 1 lesions representing aortic dissection and its variants share a diseased aorticmedia as their common pathologic lesion. Classic dissection is characterized by the development of a flow channel or false lumen within the aortic wall, whichis separated from the true lumen by a dissection membrane & #40;Fig2& #41;.
血液常常通过撕裂的内膜流向假腔,然后再通过一个或多个撕裂破口流回真腔。无论有无明确的撕裂内膜片,当假腔内新鲜血液凝固时,就可以称之为IMH或者撕裂变异。 Blood most commonly flows into the false lumen through a primary intimal tear, and re-entersthe true lumen through one or more exit tears. Regardless of the presence of an identifiable primary intimal tear, when fresh blood coagulates within a falselumen space, we refer to it as an IMH or dissection variant.
少数有中层病变的患者,出现表浅或者部分撕裂(相当于原发性内膜撕裂),但并没有形成一个单独的流出道,或者造成壁内血液的存留。这些少见的病变称之为局限撕裂或者局限性夹层,与典型夹层对比往往具有细微的影像改变(30,33,36)(图3)。 In a smallnumber of patients with medial disease, a superficial/partial thickness tear develops & #40;the equivalent of a primary intimal tear& #41; without the development ofa separate flow channel or accumulation of intramural blood. These rare lesionsare referred to as limited tears or limited dissection and tend to have subtle imaging findings when compared with classic dissection & #40;30,33,36& #41;& #40;Fig 3& #41;.
具有中层病变的患者,其病变进展迅速,以主动脉夹层,IMH和局限撕裂为特征,这些特征常常重叠出现(图5)。 In patientswith medial disease, lesions can evolve rapidly, and features of aortic dissection, IMH, and limited tears can and often do overlap & #40;Fig 5& #41;. 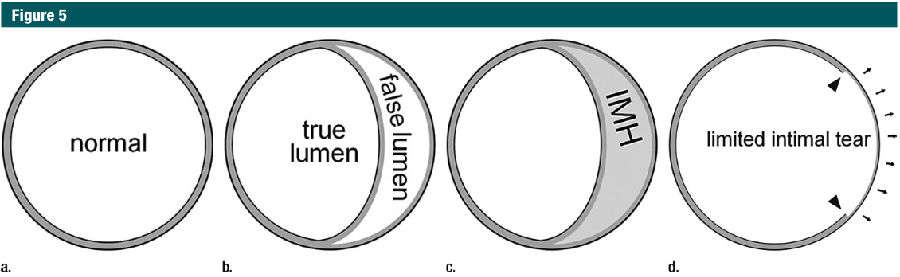
图5:主动脉夹层变异的示意图 (a)正常心脏外周胸主动脉壁的分层结构:内膜、中膜、外膜。大部分主动脉壁的结构是中层(灰色)。内膜和外膜(如图,黑色主动脉壁的内外轮廓)在CT上是不可见的。所有主动脉夹层变异都发生在主动脉壁的中层。 (b)经典的主动脉夹层发生在中层结构的外三分之一,将血流分成两个通道。注意,分隔真、假腔的组织实际是中层结构,应称之为内中膜皮瓣。 (c)当分离的中层结构中充满静止血液而非流动血液时,称为IMH。 (d)局限性内膜撕裂实际指部分撕裂(箭头)穿透内膜和中膜内层,残余的中膜/外膜暴露,这导致动脉壁圆周局限性“膨胀”(箭头)。(转载、许可、引用30)
第二组病变代表PAU,其特点是在增厚的病变内膜上,溃疡穿透了内膜的弹性层到达了主动脉壁的深层,这可能与IMH相关。伴有PAU的IMH病变通常比合并中层病变(夹层变异)的单纯IMH预后更差(37)。 Group 2 lesions representing PAUs are characterized by defects in the thickened anddiseased intima that penetrate through the internal elastic lamina into deeperlayers of the aortic wall, which may be associated with IMH. When associatedwith PAU, IMH generally has a worse prognosis than uncomplicated IMH associatedwith medial disease & #40;dissection variant& #41; & #40;37& #41;.
第三组病变是主动脉瘤破裂,最常发生在腹主动脉(图4)。不稳定动脉瘤的特征是一层慢性的血栓包裹新鲜血液(新月征),壁内出现血液和瘤周滞留。 Group 3 lesions are rupturing aortic aneurysms, occurring most frequently in the abdominal aorta & #40;Fig 4& #41;. Signs of unstable aneurysms are fresh blood within a layerof chronic thrombus & #40;crescent sign& #41;, intramural blood, and perianeurysmal stranding.
几乎所有AAS以及并发症的结构特征可以由现代CTA进行评估。这种综合形态学评估的普及为AAS自然病程提供了独特见解,可以精确分类,并有利于外科手术的实施和血管内治疗。 Virtually all structural features associated with AAS and their complications can be reliably assessed with modern CT angiography.The widespread availability of this comprehensive morphologic assessment is providing unique in- sights into the natural history of AAS, allowing refinedclassification schemes and better implementation of surgical and endovascular treatments.
|