|
本期的“跟科学家一起读文献”专栏由PKRC团队的杨俊博士为您带来CT灌注神经影像篇的分享。点击此处查看往期回顾。
杨俊 博士 加拿大医学影像博士。研究领域主要在定量影像,核医学和医学物理。归国前,在加拿大Robarts research institute 获得了博士学位并担任研究员,曾是加拿大国家研究院访问研究员。从事脑卒中,认知障碍和阿兹海默症影像和治疗的临床和试验科研工作,博士期间加入了加拿大多中心和加拿大-欧洲急性缺血性脑卒中联合项目,参与设计一站式多模态CT在急性脑卒中的影像方案。现任GE Healthcare高级应用科学家,设计并联合开发了CT灌注影像处理软件CT Kinetics(CK),致力于脑卒中多模态CT标准化以及神经影像的科研应用。
Association Between CT Angiogram Collaterals and CT Perfusion in the Interventional Management of Stroke III Trial Achala Vagal, MD. MS; Bijoy K. Menon, MD; Lydia D. Foster, MS; Anthony Livorine, MD; Sharon D. Yeatts, PhD; Emmad Qazi, BS; Chris d’ Esterre, PhD; Junzi Shi, MD; Andrew M. Demchuk, MD: Michael D. Hill, MD, MSc; David S. Liebeskind, MD; Thomas Tomsick, MD; Mayank Goyal, MD Stoke. 2016;47:535-538
点击下载或查看文献原文:  STroke2016- Association Between CT Angiogram Collaterals and CT Perfusion IMS trial.pdf STroke2016- Association Between CT Angiogram Collaterals and CT Perfusion IMS trial.pdf
CTA侧枝循环与CTP(CT灌注)缺血信息的关联性 – 对于IMS-III脑卒中临床试验的病患筛查 (ESCAPE/IMS Trial组委,加拿大卡尔加里大学) 背景简要: 在急性缺血性脑卒中(AIS)里,侧枝循环的好坏可以直接影响到缺血半暗带(tissue at risk)的大小以及核心梗死(ischemic core或infarct)的进展。AIS动脉机械取栓前,侧枝循环,缺血半暗带和核心梗死因素应该被考虑在病人的筛查和治疗方案管理中。本文在IMS-III期随机开放性试验中,利用CTP(CT灌注)和CTA(CT血管造影)的多模态CT影像,来探究CTA侧枝循环在AIS病患的机械取栓筛查中与CTP血流动力学参数的相关性。 实验方法和重要结果: 在IMS-III期试验中(总共656名试验对象),95名病患被纳入本研究,并接受多模态CT影像 (CTP+CTA)检查。基线CTA证实了53名病患具有前循环大血管闭塞,即ICA,M1及M2段闭塞。在这些患者中,同时进行的CTP检查用以分析和量化缺血半暗带,核心梗死大小和不匹配率。CTP图像全部由具备延迟不敏感算法的商业软件进行半自动处理。运动位移,动静脉输入,时间-增强动态曲线等都进行半自动处理。缺血半暗带被定义为Tmax(达峰反应时间)> 6s的区域,核心梗死被定义为Tmax> 6s 和relative CBF(相对血流速,与正常对侧相比值)小于30%的双阈值区域。通过这些阈值定义,缺血半暗带,核心梗死体积以及缺血区不匹配率被计算出来。CTA图像结果划分软脑膜的侧枝循环覆盖区域为2个灌注分区(前-中动脉区域和中-后动脉区域),每个灌注区域做6分评分(0-5分,0分最差,指示无侧枝显示;5分指示为正常或增加侧枝),CTA侧枝循环总评分为两个分区的评分总和,划分为好(总和8-10分),良(总和6-7分),差(总和0-5分)三个级别的评分。 在总共656名AIS试验患者中,104人接受了基线CTP检查,其中85人接受了CTP+CTA检查,53个病患(53/85或62.4%)被证实是大脑中动脉M1/M2段和颈内动脉ICA段闭塞。使用Kruskal-Wallis和Spearman相关性统计方法,本试验证实了good CTA collateral(侧枝循环评分8-10分)病人具有较小的核心梗死体积和较大的不匹配区域比例。其中侧枝循环评分与梗死核心大小呈中度负相关,而与不匹配区域的缺血半暗带指针呈正相关。低灌注区域体积(hypoperfused volume)与侧枝循环状态尚未显示足够关联性(Table 2及图例)。核心梗死大小未能区分好与良,良与差之间的侧枝循环状态。
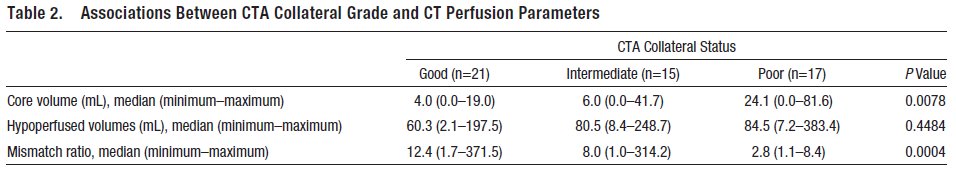 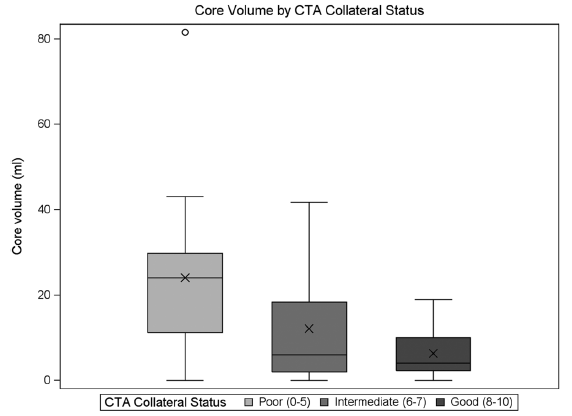
结论: 良好的CTA侧枝循环能够反映较好的CTP不匹配比例和较低的核心梗死体积的关联性。通过其相关性,CTA与CTP都可以反映出关于缺血组织的生物活性状态。 原文Abstract: Background and Purpose—Collateral flow can determine ischemic core and tissue at risk. Using the Interventional Management of Stroke (IMS) III trial data, we explored the relationship between computed tomography angiogram (CTA)collateral status and CT perfusion (CTP)parameters. Methods—Baseline CTA collaterals were trichotomized as good, intermediate, and poor, and CTP studies were analyzed to quantify ischemic core, tissue at risk, and mismatch ratios. Kruskal–Wallis and Spearman tests were used to measure the strength of association and correlation between CTA collaterals and CTP parameters. Results—A total of 95 patients had diagnostic CTP studies in the IMS III trial. Of these, 53 patients had M1/M2 middle cerebral artery±intracranial internal carotid artery occlusion, where baseline CTA collateral grading was performed. CTA collaterals were associated with smaller CTP measured ischemic core volume (P=0.0078)and higher mismatch (P=0.0004) There was moderate negative correlation between collaterals and core (rs=−0.45; 95% confidence interval, −0.64 to −0.20)and moderate positive correlation between collaterals and mismatch (rs=0.53; 95% confidence interval, 0.29–0.71) Conclusion—Better collaterals were associated with smaller ischemic core and higher mismatch in the IMS III trial. Collateral assessment and perfusion imaging identify the same biological construct about ischemic tissue sustenance. 点击下载或查看文献原文:  STroke2016- Association Between CT Angiogram Collaterals and CT Perfusion IMS trial.pdf STroke2016- Association Between CT Angiogram Collaterals and CT Perfusion IMS trial.pdf
Volume Perfusion CT Imaging of Cerebral Vasospasm: Diagnostic Performance of Different Perfusion Maps Ahmed E. Othman· Saif Afat· Omid Nikoubashman· Marguerite Muller· Gerrit Alexander Schubert· George Bier· Marc A. Brockmann· Martin Wiesmann· Carolin Brockmann Neuroradiology & #40;2016& #41; 58:787-792 点击下载或查看文献原文:  (NR-2016)VCTP of cerebral vasospasm- diagnostic performance of different perfusion maps.pdf (NR-2016)VCTP of cerebral vasospasm- diagnostic performance of different perfusion maps.pdf
蛛网膜下腔出血后的血管痉挛CTP(CT灌注)影像 – CTP灌注图像的诊断性能评估 背景简要: 大脑血管痉挛通常会出现在破裂动脉瘤造成的蛛网膜下腔出血(SAH)之后,并引起迟发性脑缺血(delayed cerebral ischemic-DCI),DCI会造成更严重的神经机能和认知缺失。血管痉挛有可能发生在SAH之后的第2-14天内,所以尽早的探测/预测出现血管痉挛的这类病人,在治疗和病人预后管理中至关重要。CTP(CT灌注)影像能够提供多种定量的血流动力学信息,可用以监测早期血管痉挛。本试验利用CTP成像,评估了不同定量参数对SAH病人出现血管痉挛的诊断性能。 实验方法和重要结果: 在本试验中,从2011年3月到2014年5月一共纳入了26名因动脉瘤破裂引起的SAH病人(6.7±2.6天后),这些病人都在发现症状6小时内接受了CTP和DSA。其中10个动脉瘤位于前交通动脉,7个位于大脑中动脉,5个位于颅内颈内动脉,4个位于基底动脉上。每个病患都实施了动脉瘤弹簧圈和夹闭手术,其中10个病患具有多个动脉瘤。VPCT(CT灌注)扫描在40层Siemens Somatom AS CT上进行,造影剂团注和盐水追注速率为5mL/s。覆盖长度96mm,180mAs,80kV,以1.5s时间分辨率进行45s动态采集。层厚重建为10mm。定量参数CBF,CBV,MTT,TTD均由西门子公司去卷积算法得出。TTD被定义为TTS+MTT(起始时间+平均通过时间)。半自动图像分割,图像运动校正,大血管移除都由软件完成。动脉输入函数在大脑前动脉,静脉函数取为矢状静脉窦,然后进行计算。CTP图像参数CBF,CBV,MTT和TTD用以诊断是否出现因血管痉挛引起的灌注异常,每个责任血管灌注区域被两位神经影像医师独立评估,并划分为3分Likert量表(0分-无血管痉挛影响,1分-血管痉挛影响小于50%的血管灌注区域,2分-血管痉挛影响超过50%血管区域)。所有CT平扫已经呈现梗死的血管区域都被排除。第三位放射医师评估了DSA的16段颅内主要血管的3分Likert量表(0分-无血管痉挛影响血管直径,1分-血管痉挛影响小于血管直径50%的狭窄,2分-血管痉挛影响超过血管直径的50%)。在探测血管痉挛方面,如Table 2所示,ROC曲线分析发现TTD具有最高的诊断准确性(AUC面积0.832,敏感度0.737,特异度0.928),其次诊断性能较好的为MTT和CBF。TTD与MTT的准确性明显高于CBF和CBV。CBF的准确性高于CBV(Figure 1)。而TTD的探测血管痉挛的准确性与MTT无显著统计学差异,但是McNemar检验证实了TTD的敏感度要高于MTT。所有CTP定量参数指示的血管痉挛的严重性,均与DSA的结果相关。TTD与血管痉挛Likert分数的相关性最高(R=0.685),MTT仅次于TTD。所有CTP定量参数在Cohen Kappa检验中均显示出很好的一致性(inter-rater agreement 0.927 – 1.0)。 结论: 实验结果指示CTP的TTD参数具有最高的敏感度用以探测SAH之后的血管痉挛,并在评估血管痉挛严重性上与DSA最好的相关性。
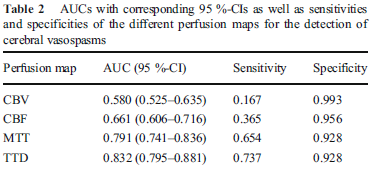
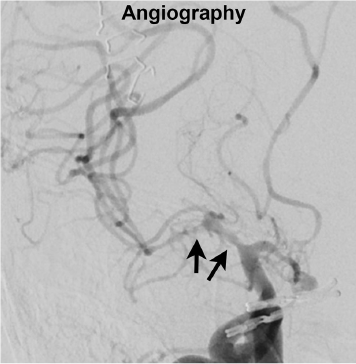
Figure 1:58岁病患在动脉夹放置后第5天出现的血管痉挛(DSA)。CTP图像参数显示异常灌注出现于右侧MCA区域(TTD最为明显,CBV指示不清晰)。 原文Abstract: Introduction—In this study, we aimed to evaluate the diagnostic performance of different volume perfusion CT (VPCT) maps regarding the detection of cerebral vasospasm compared to angiographic findings. Methods—Forty-one datasets of 26 patients (57.5 ± 10.8 years, 18 F) with subarachnoid hemorrhage and suspected cerebral vasospasm, who underwent VPCT and angiography within 6h, were included. Two neuroradiologists independently evaluated the presence and severity of vasospasm on perfusion maps on a 3-point Likert scale (0—no vasospasm, 1—vasospasm affecting <50 %, 2—vasospasm affecting >50 % of vascular territory).A third neuroradiologist independently assessed angiography for the presence and severity of vasospasm on a 3-point Likert scale (0—no vasospasm, 1—vasospasm affecting < 50 %, 2—vasospasm affecting > 50 % of vessel diameter).Perfusion maps of cerebral blood volume (CBV), cerebral blood flow (CBF),mean transit time (MTT), and time to drain (TTD) were evaluated regarding diagnostic accuracy for cerebral vasospasm with angiography as reference standard. Correlation analysis of vasospasm severity on perfusion maps and angiographic images was performed. Furthermore, inter-reader agreement was assessed regarding findings on perfusion maps. Results—Diagnostic accuracy for TTD and MTT was significantly higher than for all other perfusion maps (TTD, AUC=0.832; MTT, AUC= 0.791; p<0.001).TTD revealed higher sensitivity than MTT (p=0.007).The severity of vasospasm on TTD maps showed significantly higher correlation levels with angiography than all other perfusion maps (p ≤ 0.048). Inter-reader agreement was (almost). perfect for all perfusion maps (kappa≥ 0.927). Conclusion—The results of this study indicate that TTD maps have the highest sensitivity for the detection of cerebral vasospasm and highest correlation with angiography regarding the severity of vasospasm.
点击下载或查看文献原文:  (NR-2016)VCTP of cerebral vasospasm- diagnostic performance of different perfusion maps.pdf (NR-2016)VCTP of cerebral vasospasm- diagnostic performance of different perfusion maps.pdf
|